Immediacy is … Confidence from Day One
Where Science, Surface, Stability and combine, the BioHorizons Camlog Group provides clinically proven implant systems engineered for primary stability, biological integration, and long-term success in every immediate possibility.
Clinical advantages of implants for immediate placement
Patient-centered care paired with remarkable efficiency
Dr. Alvaro Blasi, Dr. Gonzalo Blasi and Dr. Ricardo Palacios, Barcelona, Spain
Immediate implant placement and soft tissue augmentation in a compromised lateral incisor case using a fully guided workflow
Treatment time: 4 months
Tooth numbers: 12
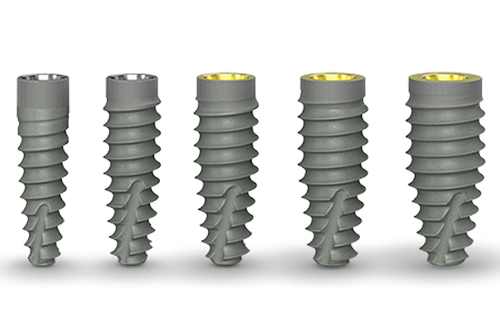
Treatment type: Immediate implant placement in the anterior zone using a CONELOG® PROGRESSIVE-LINE implant, with grafting and temporisation.
Products used: CONELOG® PROGRESSIVE-LINE implant, MinerOss® X
A patient presented with a horizontal fracture of the upper left lateral incisor (tooth 1.2), with no clinical signs of suppuration or bleeding. The periodontal phenotype was thin, and the buccal bone wall was minimally thick, increasing the risk of soft tissue recession following extraction. A minimally invasive and digitally planned treatment was chosen to preserve tissue architecture and ensure a predictable aesthetic result.
This case demonstrates that immediate implant placement with simultaneous bone and soft tissue grafting, supported by a guided protocol and digital planning, can deliver stable, aesthetic and predictable results even in challenging thin biotype scenarios.
Treatment planning and diagnosis
A CBCT and intraoral scans assessed the site, and coDiagnostiX® software was used to plan implant positioning and design the surgical guide virtually. The plan included immediate implant placement, filling the buccal gap with a xenograft and a soft tissue graft from the maxillary tuberosity to enhance soft tissue thickness in this high-risk aesthetic area.
Surgery and initial outcomes
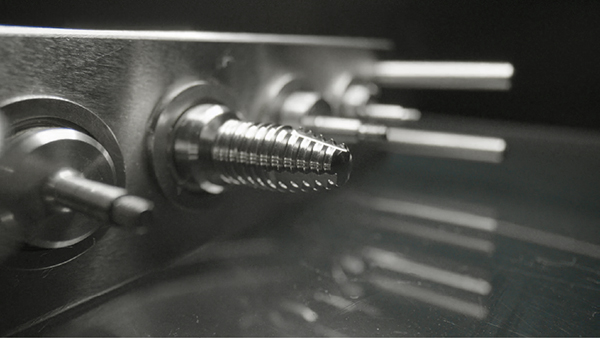
A minimally invasive extraction was performed using the Benex® system to preserve the thin buccal bone. A 3.3 x 11 mm CONELOG PROGRESSIVE-LINE implant was placed using a fully guided protocol. Despite the narrow implant diameter, a torque of 20 Ncm was achieved, facilitated by good palatal bone availability, under-preparation of the osteotomy and the macro design of the implant. The peri-implant gap was grafted with MinerOss X, chosen for its slow resorption profile and volume-stabilising characteristics. A connective tissue graft was harvested from the tuberosity by performing a distal wedge in the region of tooth 1.8. The graft was secured in a buccal pouch using a horizontal mattress suture with 6-0 polypropylene to support the emergence profile and soft tissue volume. A customised healing abutment was placed to seal the socket and guide soft tissue healing. A provisional resin-bonded restoration was applied out of occlusion.
Main clinical outcomes
Four months post-placement, the implant site exhibited stable soft tissue contours and full graft integration. A screw-retained lithium disilicate crown was delivered and bonded to a customised anodised titanium abutment. Radiographs confirmed excellent osseointegration and bone preservation. Post-operative care included chlorhexidine 0.12% gel application twice daily for 14 days. The patient expressed high satisfaction with the aesthetic result, and no recession or tissue shrinkage was observed during the healing period.
Benefits of chosen solutions
The chosen treatment approach provided several clinical advantages. The fully guided protocol using coDiagnostiX software allowed for precise and minimally invasive implant placement, which was particularly beneficial given the thin buccal bone anatomy. Grafting with MinerOss X helped to maintain buccal contour and support volume stability in the thin periodontal phenotype. Using a connective tissue graft harvested from the tuberosity further enhanced soft tissue thickness and it was placed with minimal trauma using horizontal mattress sutures for secure adaptation. A customised healing abutment and staged provisionalisation supported controlled soft tissue maturation during healing. Finally, the restoration was completed with a screw-retained ceramic crown on a customised anodised titanium abutment, providing long-term stability and a highly aesthetic result.
Dr. Ramon Gomez Meda, Ponferrada, Spain
Restoring a central incisor without compromising soft or hard tissue volume
Treatment time: 30 minutes
Tooth numbers: 11
Treatment type: Immediate implant placement in the anterior zone, with grafting and temporisation.
Products used: CONELOG® PROGRESSIVE-LINE implant, MinerOss® XP
A 67-year-old female patient presented with a broken central incisor. The tooth in question had been restored with a crown several years ago, but this had since detached. The patient did not report being in pain, though she was concerned about the appearance of her smile. Her initial assessment revealed no relevant medical history and she was a non-smoker.
Successful implant placement was achieved with a simultaneous fixed temporary restoration in this case. In doing so, the aesthetic and functional demands of the patient were fulfilled without compromising their long-term biological needs.
Treatment planning and diagnosis
An intraoral scan and a CBCT image were acquired as part of the comprehensive assessment. The images were matched using dental Blue Sky Bio software to facilitate the design of the surgical guide, using a prosthetically-driven planning approach to find the ideal 3D position of the implant. The surgical template was 3D printed and sterilised in preparation for surgery.
Surgery and initial outcomes
The remaining root was carefully and atraumatically extracted using a Benex® pull-out device. The surgical guide was fitted in the mouth and a CONELOG PROGRESSIVE-LINE implant with conical connection was immediately placed, torqued to above 50 Ncm for high primary stability. The space between the implant and the facial cortical bone plate was filled with MinerOss XP biomaterial and a connective tissue graft was tunnelled around the neck of the implant. This was harvested from the tuberosity, de-epithelialised, and added around the neck of the implant. The objective of this procedure was to ensure long-term papilla stability and prevent both the future collapse of the soft tissue and opening of the embrasures. This is paramount when restoring a gap in the anterior zone.
A scanbody was used to register the implant position and a provisional restoration was designed in exocad software and milled in PMMA. The temporary restoration would be used to help stabilise the connective tissue graft, while also shaping the soft tissues to develop a good emergence profile. This is an important transition stage before the final restoration.
Main clinical outcomes
Surgical healing was uneventful and the patient reported no pain or discomfort. Papillae remained healthy and filled the embrasures completely. A final zirconia restoration was ultimately placed, designed to slightly alter the over-contoured emergence profile from the exocad software. This simplified the fitting protocol and further prevented the collapse of the hard or soft tissue during the final healing phase.
Benefits of chosen solutions
Immediate loading provides aesthetic, functional and biological advantages. The CONELOG PROGRESSIVE-LINE implant was selected for this case because it supports immediacy by facilitating high primary stability. MinerOss XP is my preferred bone substitute in immediate cases because of its handling and low rate of resorption.